Knee pain can make everyday tasks, such as walking up and downstairs, considerably more difficult and uncomfortable. In this article, we’ll help you understand how knee anatomy and function play a role in knee pain, explore common causes, and learn how to assess your own condition. We’ll also discuss at-home remedies, physical therapy exercises, alternative treatments, and medical interventions to provide you with effective strategies for managing knee pain and regaining mobility.
Understanding Knee Anatomy and Function
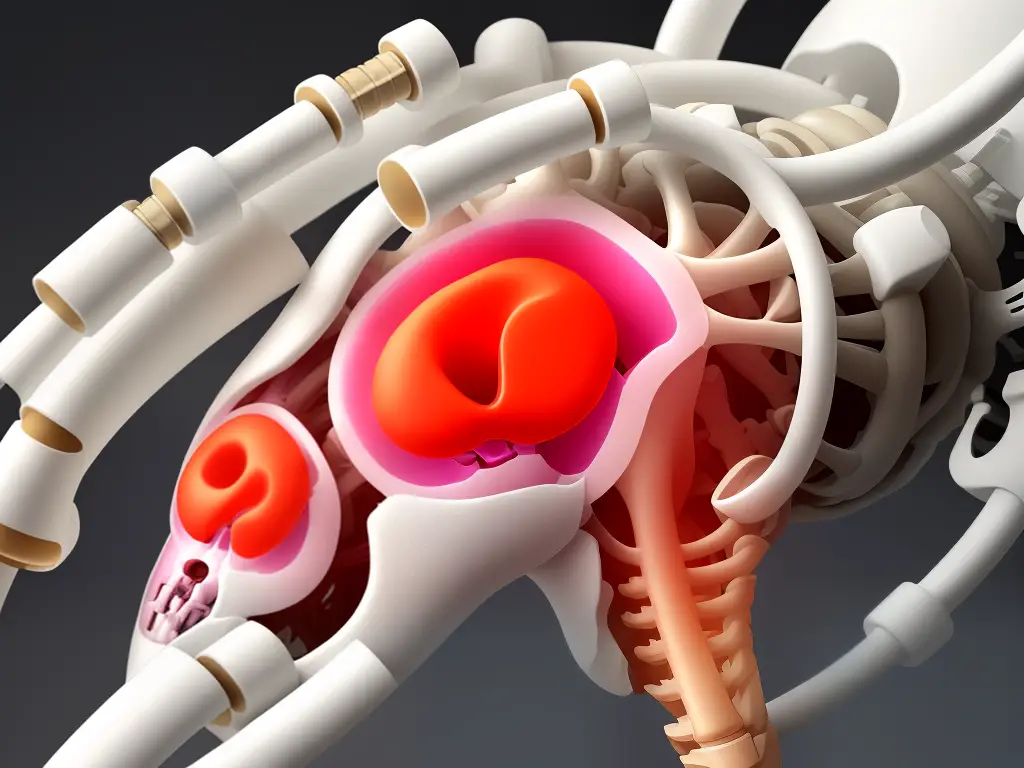
The knee joint is a complex structure that connects your thigh bone (femur) to your shin bone (tibia). It consists of several essential components, including muscles, ligaments, cartilage, and tendons.
- Bones: The main bones in the knee joint are the femur, tibia, and patella (kneecap). These bones provide structure and stability to the joint.
- Muscles: Quadriceps and hamstrings are the main muscle groups involved in knee movement. The quadriceps help straighten the knee, while the hamstrings help bend it.
- Ligaments: These are strong, fibrous connective tissues that connect bone to bone and provide stability. The four main ligaments in the knee are the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL).
- Cartilage: There are two types of cartilage in the knee joint: articular and meniscus. Articular cartilage is a smooth, slippery material that covers the ends of the femur and tibia, allowing them to glide easily against each other. Menisci are C-shaped pieces of cartilage that act as shock absorbers between the femur and tibia, helping to distribute weight evenly across the joint.
- Tendons: These are strong, flexible connective tissues that attach muscle to bone. The quadriceps tendon connects the quadriceps muscle to the patella, while the patellar tendon connects the patella to the tibia.
The muscles, ligaments, cartilage, and tendons in the knee joint work together to provide stability, flexibility, and shock absorption.
- Muscles contract and relax to create movement in the joint. The quadriceps extend the knee, while the hamstrings flex it.
- Ligaments help stabilize the joint by limiting excessive movement, such as twisting or bending too far.
- Cartilage, particularly meniscus, aids in shock absorption and even distribution of weight across the joint to minimize stress on the bones.
- Tendons transfer force from muscles to the bones, allowing the knee to move and support weight.
It’s important to note that some stairs-related knee pain may arise from imbalances or overuse of certain muscles, added strain on ligaments, or wear and tear of the cartilage.
Several common injuries or overuse conditions can cause knee pain when going up and down stairs:
- Patellofemoral pain syndrome: Pain at the front of the knee due to incorrect tracking of the patella over the femur, often causing inflammation and irritation in the soft tissues around the joint.
- Meniscus tear: A tear or rupture in the menisci can cause pain, especially when bending the knee, as the damaged cartilage rubs against the adjacent joint surfaces.
- Tendinitis: Inflammation of the tendons surrounding the knee joint, such as the quadriceps and patellar tendons, can lead to pain and reduced mobility.
- Ligament injuries: Damage to the ACL, PCL, MCL, or LCL can result in pain, instability, and weakness in the knee joint, particularly during activities like walking up or down stairs.
If you’re experiencing knee pain when using stairs, several treatment options may be helpful:
- Rest: Taking a break from activities that worsen knee pain, such as stair climbing, can help alleviate symptoms and facilitate healing.
- Ice: Apply ice packs to the affected knee area for 15-20 minutes at a time, several times a day, to reduce pain and inflammation.
- Compression: Use a knee brace or wrap to provide support and reduce swelling.
- Elevation: Keep your leg elevated when resting to help minimize swelling and accelerate healing.
- Physical therapy: A physical therapist can provide you with targeted exercises to strengthen the muscles supporting the knee joint, improve flexibility, and correct any muscle imbalances that may be contributing to your pain.
- Medications: Over-the-counter pain relievers and anti-inflammatory medications, such as ibuprofen or naproxen, can help manage pain and inflammation.
Always consult a healthcare professional for personalized advice based on your specific symptoms and conditions. If conservative treatments fail to provide relief or your knee pain worsens, you may need to discuss alternative interventions with your healthcare provider, potentially including injections or surgery.

Causes of Knee Pain and Treatment for Knee Pain when using Stairs
Arthritis is a common cause of knee pain and includes different types such as osteoarthritis, rheumatoid arthritis, and gout. Ligament injuries can occur from sports or physical activities, particularly in tears of the ACL, PCL, or MCL. Patellar tracking disorder can cause pain when walking up and downstairs, and it can be due to muscle imbalances or even a misshapen patella. Meniscus tears are another cause that often occurs with aging, causing pain, swelling, and stiffness. Lastly, bursitis occurs in overuse, injury, or infection, creating inflammation and difficulty to move the knee.
Reducing activities that cause pain, applying ice packs to the affected area, and compression bandages are recommended for relieving knee pain. Elevating the affected limb can decrease swelling and inflammation. Over-the-counter pain medication, exercise, and weight management can also provide relief. In some cases, corticosteroid injections, physical therapy, or surgery may be necessary, depending on the cause of knee pain. It is important to consult with a healthcare professional for proper assessment and treatment plan.

Assessing Your Own Condition: Knee Pain Stairs Treatment
Step 1: Identify the symptoms
- Pain in the knee while using stairs (going up or down)
- Swelling or inflammation around the knee joint
- Stiffness or a reduced range of motion in the knee
- Popping or cracking noises while using the stairs
- Feeling of instability or the knee giving way
Step 2: Determine the severity and frequency of the pain
- Is the pain mild, moderate, or severe?
- Does your knee pain occur every time you use stairs or only occasionally?
- Have you noticed any patterns or specific triggers that make the pain worse?
- Is the pain worse during certain times of the day?
Step 3: Identify potential contributing factors
- Previous knee injuries or surgeries
- Overuse or strain from physically demanding activities or sports
- Obesity or being overweight, which puts extra stress on the knee joint
- Poor footwear or walking/running on uneven surfaces
- Age-related wear and tear, such as arthritis
Step 4: Try at-home remedies and self-care
- Rest your knee and avoid using stairs as much as possible.
- Apply ice packs to the affected area for 15-20 minutes every few hours.
- Use over-the-counter pain relievers, such as ibuprofen, to reduce inflammation and pain.
- Elevate your leg and consider using a knee brace for added support.
- Gently stretch and strengthen the muscles around your knee through low-impact exercises.
Step 5: Recognize when it’s time to consult a medical professional
- Severe pain or swelling that doesn’t improve with at-home remedies
- Decreased range of motion or inability to bear weight on the affected leg
- Signs of infection, such as redness, warmth, and fever
- Pain that affects your daily activities and overall quality of life.
A healthcare provider can help determine the root cause of your knee pain and develop an appropriate treatment plan to ensure your knee health and stability moving forward.

At-home Remedies and Treatments for Knee Pain when using Stairs
Knee pain while walking upstairs can be a hindrance to your daily activities, but there are several non-surgical methods to alleviate the pain. Here are some at-home treatments and remedies to help reduce knee pain and make walking up and down the stairs more comfortable and less painful:
- Over-the-counter anti-inflammatory medications: Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help control inflammation and relieve knee pain when using stairs. Always follow the recommended dosage on the label and consult with your healthcare provider if you have any questions about these medications.
- Heat and ice therapy: Alternating between heat and cold packs can help soothe the pain and reduce inflammation in the knee. Apply a cold pack to your knee for 20 minutes, then wait for an hour and apply a heat pack for another 20 minutes. Repeat this process several times throughout the day, as needed.
- Rest: Give your knee adequate time to rest and recover, especially if your pain is due to overuse or a recent injury. Avoid activities that cause further pain or discomfort, and consider using a cane or crutches to take the pressure off your knee when using stairs.
- Stretching and strengthening exercises: Gentle exercises focused on improving the flexibility and strength of your quadriceps, hamstrings, and calf muscles can help alleviate knee pain. Speak with a physical therapist about which exercises are appropriate for your specific knee condition. Examples of helpful exercises may include calf stretches, hamstring stretches, or straight leg raises.
- Elevation: Elevate your knee above heart level when resting to help decrease inflammation and facilitate healing.
- Knee braces and compression sleeves: Wearing a supportive knee brace or compression sleeve can provide added support and reduce pain when walking upstairs. Choose a brace that is comfortable and provides adequate support for your specific knee condition. Consult with a healthcare professional for advice on selecting the best brace or sleeve for your needs.
- Weight management: Maintaining a healthy weight can reduce the amount of stress and pressure on your knee joints when using stairs. If you are overweight, talk with your healthcare provider about a safe and effective weight loss plan that includes diet and exercise.
- Shoe inserts: If your knee pain is due to foot mechanics or alignment issues, shoe inserts or orthotics may help alleviate the pain and improve your gait. Speak with a podiatrist or orthotic specialist to determine if inserts could benefit you.
Remember, it is important to consult with your healthcare provider before starting any new treatments or exercise routines. They can evaluate your specific situation and recommend the best course of action to manage your knee pain when using stairs.

Knee Pain Stairs Treatment: Physical Therapy and Exercise for Adults
Knee pain while climbing or descending stairs is a common complaint among adults. This discomfort may be due to various causes such as arthritis, overuse, muscle imbalances, or injury. Physical therapy exercises and stretches can help alleviate knee pain and provide support for the surrounding muscles and joints, reducing the risk of future injuries. This guide will outline the proper techniques and recommended exercises for addressing your knee pain during stair-climbing.
Consult a Healthcare Professional: Before beginning any exercise or physical therapy program, consult your healthcare provider to ensure that these exercises are appropriate for your specific condition. They may recommend an evaluation by a physical therapist who will design a personalized treatment plan.
Warm-Up: Prepare your muscles for exercise by engaging in light activities such as walking, cycling, or using an elliptical trainer for about 10 minutes. Warming up can help to reduce the risk of injury during your exercise routine.
- Exercises:
- Quad Stretch:
- Stand upright and hold onto a wall or chair for balance.
- Bend your right knee and grab your right ankle with your right hand.
- Gently pull your ankle towards your buttocks, feeling the stretch in your quadriceps (front of thigh).
- Hold for 30 seconds and repeat on the left side.
- Aim to perform 2-3 sets on each side.
- Hamstring Stretch:
- Sit on the floor with both legs extended in front of you.
- Slowly bend your left knee, placing the sole of your left foot against your right inner thigh.
- Reach forward with both hands, trying to touch your right foot.
- Hold the stretch for 30 seconds, then repeat on the other side.
- Aim to perform 2-3 sets on each side.
- Calf Stretch:
- Stand facing a wall, with your hands resting on the wall.
- Step back with your right foot, keeping your right knee straight and your right heel on the floor.
- Lean forward, feeling the stretch in your right calf.
- Hold for 30 seconds and repeat on the left side.
- Aim to perform 2-3 sets on each side.
- Straight Leg Raises:
- Lie on your back with your left knee bent and your right leg extended.
- Tighten your right thigh muscles and lift your right leg straight up, keeping your toes pointed toward the ceiling.
- Hold for a few seconds before slowly lowering your leg back down.
- Complete 10-15 repetitions for 2-3 sets, then switch legs.
- Clamshells:
- Lie on your left side with your knees bent to 90 degrees and your feet together.
- Keeping your feet together, lift your right knee as high as you can without moving your pelvis.
- Slowly lower your knee back to the starting position.
- Perform 10-15 repetitions for 2-3 sets, then switch sides.
- Step-Ups:
- Stand in front of a stable step platform or staircase.
- Place your right foot on the step, then press through your right heel to lift your body up.
- Slowly lower back down to the starting position.
- Perform 10-15 repetitions for 2-3 sets, then switch legs.
- Wall Squats:
- Stand with your back against a wall, feet hip-width apart, and about 2 feet away from the wall.
- Slide down the wall, lowering your body until your thighs are parallel to the ground.
- Hold for 10-30 seconds, then slowly slide back up to the starting position.
- Aim to perform 2-3 sets.
Cooldown: Conclude your exercise routine with a cooldown period of light activity—such as walking or cycling—for about five minutes. Follow this with gentle stretches for all major muscle groups to maintain flexibility.
Monitor Your Progress: As your strength and flexibility improve, you may increase the intensity, repetitions, or sets of these exercises. Maintain a consistent routine and follow your healthcare provider’s or physical therapist’s recommendations for progress assessments.
Remember, consistency is key to achieving your knee pain stairs treatment goals. Always listen to your body and consult your healthcare professional if your knee pain persists or worsens.

Alternative Treatments for Knee Pain Relief When Using Stairs
Acupuncture is an ancient Chinese practice that involves inserting fine needles into specific points (called acupoints) on the body to stimulate natural healing and pain relief. Research has shown that acupuncture can be effective in reducing knee pain, especially for those who suffer from osteoarthritis-related knee pain.
- Consult a licensed acupuncturist with experience in treating knee pain
- Attend a few acupuncture sessions for the best results
- Follow any aftercare advice provided by the acupuncturist, including specific stretches or self-massage techniques
Visiting a chiropractor can help address joint misalignments, which may be contributing to knee pain. Chiropractic care involves joint manipulation and manual therapy to help ease pain and restore function.
- Seek out a licensed chiropractor trained in treating knee pain
- Attend regular chiropractic appointments as recommended by the practitioner
- Discuss any concerns you have about your knee pain with your chiropractor and follow their advice regarding additional exercises and therapies
Massage therapy can help to alleviate muscle tension, reduce inflammation, and promote relaxation, which can be beneficial for knee pain relief. Targeted massage for the muscles surrounding the knee can provide relief and help to improve overall joint function.
- Consult a professional massage therapist who specializes in treating clients with knee pain
- Schedule regular massage sessions tailored to your needs and preferences
- Discuss with your therapist about specific techniques and massage styles that can provide the most relief for your knee pain, such as Swedish massage, deep tissue, or trigger point therapy
Physical therapy is a crucial component in treating knee pain, especially if your knee pain is due to an injury or chronic condition. A physical therapist will work with you to create a personalized exercise program to help strengthen supporting muscles, increase flexibility, and improve overall knee function.
- Seek a qualified physical therapist experienced in treating knee pain and injuries
- Attend regular therapy appointments and diligently follow the prescribed exercise program at home
- Communicate with your physical therapist about your progress and any concerns or questions you may have
In addition to the above treatments, certain herbal and nutritional supplements can help alleviate knee pain. Consult a professional like a naturopathic doctor or nutritionist for personalized recommendations.
- Consult with a professional who can provide guidance on herbal and nutritional supplements
- Research supplements such as glucosamine, chondroitin, and turmeric, which have anti-inflammatory properties and can support joint health
- Follow the recommended dosage and consult your healthcare provider before starting any new supplement to avoid potential interactions with medications or pre-existing conditions
Remember that consistency and patience are essential when trying alternative treatments for knee pain. It may take time to see significant improvements, and combining multiple therapies may be necessary to achieve optimal results. Always check with your healthcare provider before starting any new treatment or therapy to ensure it is safe and appropriate for your specific circumstances.

Medical Interventions for Knee Pain: When and How to Seek Treatment
Knee pain is a common issue that can impact adults of all ages and activity levels. While some knee pain can be managed through at-home remedies and lifestyle modifications, there may be instances where medical intervention is necessary.
When to Seek Medical Intervention for Knee Pain
Be sure to consult a healthcare professional if your knee pain presents any of the following symptoms:
- Severe pain that prevents you from bearing weight on the affected leg.
- Swelling around the knee that persists for more than 48 hours.
- Persistent pain that does not improve after a few weeks of rest, ice, compression, and elevation (RICE) treatment.
- Presence of fever or warmth around the knee, which can be indications of an infection.
- Inability to fully extend or flex the knee joint.
- Popping, clicking, or grinding sounds and sensations when moving the knee.
- A fall or injury that causes deformity around the knee joint or severe pain and swelling.
Range of Treatments Available
Depending on the severity and cause of the knee pain, there are various treatment options that your healthcare professional may recommend:
- Medications: Over-the-counter pain relievers, such as ibuprofen or naproxen, can help ease pain and reduce inflammation. In some cases, a prescription-strength medication may be necessary.
- Physical therapy: A physical therapist can teach you exercises and stretches to help improve flexibility, strength, and stability, which may help alleviate knee pain and prevent future issues.
- Orthotics: Shoe inserts, knee braces, or supportive devices can provide additional support and relieve pressure on the knee joint.
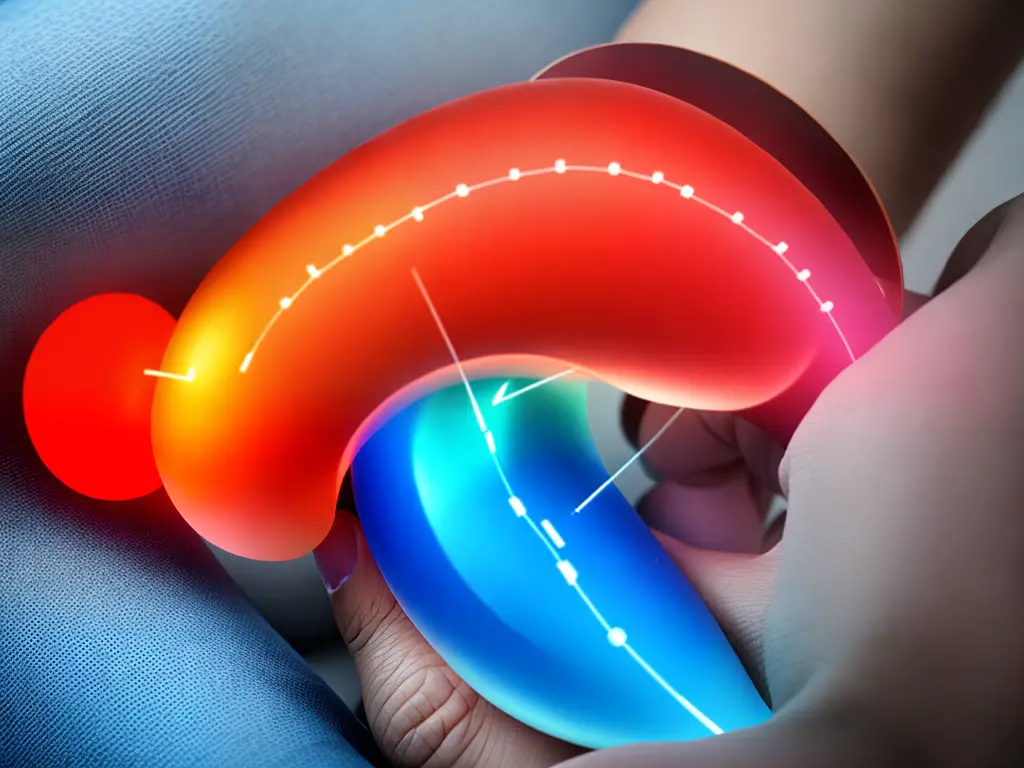
- Corticosteroid injections: In some instances, a corticosteroid injection may be administered to reduce inflammation and provide temporary pain relief.
- Hyaluronic acid injections: These injections help lubricate the knee joint by supplementing the natural synovial fluid, which can relieve pain and improve joint function.
- Platelet-rich plasma (PRP) treatment: This procedure involves injecting a patient’s own platelet-rich plasma into the knee joint to promote healing and relieve pain.
Surgical Options and Criteria for Surgery
In more severe cases or when conservative treatments have failed, surgery may be considered as a treatment option:
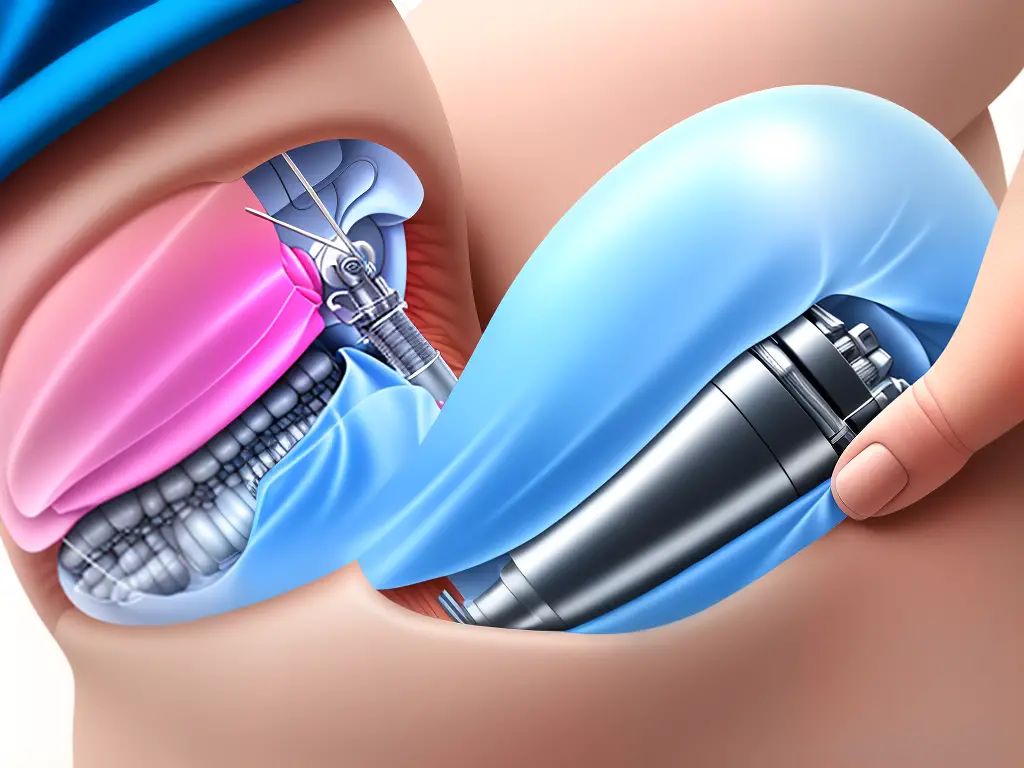
- Arthroscopy: This minimally invasive surgery involves inserting a small camera and instruments through tiny incisions to diagnose and treat various knee issues.
- Meniscus repair: If a torn meniscus is causing knee pain, this surgical procedure involves repairing or removing damaged tissue.
- ACL reconstruction: This involves replacing a torn anterior cruciate ligament (ACL) with a graft to restore knee stability and function.
- Partial knee replacement: Damaged or diseased parts of the knee are replaced with artificial components, offering relief from pain and improved function.
- Total knee replacement: In more severe cases where the entire knee joint is affected, a total knee replacement surgery may be necessary.
To determine if surgery is necessary, your healthcare professional may consider the following criteria:
- Severity and duration of pain: If knee pain severely impacts your quality of life and has not improved with conservative treatments, surgery may be recommended.
- Degree of joint damage: If the knee joint has considerable damage, surgery may provide the best chance for long-term relief.
- Age and activity level: Younger patients and those engaged in high-intensity activities may require surgery to maintain their desired level of activity.

Armed with this knowledge, you can take action to effectively manage and treat your knee pain. Remember, it’s crucial to know when to seek professional medical advice, and always consult with a medical professional before starting any exercise or treatment program. With the right strategies in place, you can work towards reducing knee pain and maintaining a healthy and active lifestyle.